- Pradhan Mantri Jan Arogya Yojna (PMJAY) was launched in September 2018 by the Prime Minister of India, Shri Narender Modi.
- PMJAY covers most medical costs, including treatments, medicines, tests, and even pre-hospital expenses.
- It aims to provide health insurance coverage of Rs. 5 lakhs per family per year for secondary and tertiary care hospitalisation.
- The scheme benefits over 12 crore poor and vulnerable families (around 55 crore people).
- Can apply for the scheme and check eligibility for Ayushman Bharat through the official website or through Paytm App.
To make healthcare insurance and other medical related services more accessible irrespective of class, caste, age or gender, the Government of India has launched PMJAY in September 2018. The full form of PMJAY is Pradhan Mantri Jan Arogya Yojna. Considered as one of the world’s largest healthcare schemes, PMJAY covers most medical costs, including treatments, medicines, tests, and even pre-hospital expenses. This scheme aims at providing financial support to majorly the bottom 40% of India’s population (approx 55 crore Indian citizens), thus making healthcare more accessible by everyone at any time.
Through this comprehensive blog, we’ll explore the meaning of the PMJAY scheme, its key features, eligibility criteria along with the procedure of applying for availing this beneficial scheme. Paytm app has also contributed significantly in making it easier for people to access various healthcare services such as creating a health ID, scheduling lab tests, purchasing health insurance, applying for medical loans, and even checking eligibility for Ayushman bharat PMJAY scheme.
What is PMJAY (Ayushman Bharat Yojana)?
Launched on 23 September 2018 in Ranchi, Jharkhand by the Hon’ble Prime Minister of India, Shri Narendra Modi, Pradhan Mantri Jan Arogya Yojna (PMJAY) is the world’s largest health assurance scheme and is one of the components of Ayushman Bharat. PMJAY was previously called the National Health Protection Scheme (NHPS) before it was renamed. It replaced the Rashtriya Swasthya Bima Yojana (RSBY), which started in 2008. Families that were covered under RSBY are also included in PMJAY, even if they are not listed in the 2011 SECC database. The scheme is fully funded by the government, with the costs shared between the Central and State governments.
It aims to provide health insurance coverage of Rs. 5 lakhs per family per year for secondary and tertiary care hospitalisation to over 12 crores of poor and vulnerable families. These approximately 55 crore Indian citizens constitute the bottom 40% of India’s population and are provided with financial support for hospital expenses during medical emergencies.
What are the Key Features of Ayushman Bharat Yojana Scheme?
- It offers coverage of ₹5 lakh per family per year for secondary and tertiary hospital care in both public and private hospitals across India.
- The scheme benefits over 12 crore poor and vulnerable families (around 55 crore people).
- Allows beneficiaries to access cashless healthcare services directly at the hospital.
- It covers up to 3 days before hospitalization and 15 days after, including diagnostics and medicines.
- There are no limits on family size, age, or gender, and all pre-existing conditions are covered from the first day.
- The scheme is portable, meaning beneficiaries can receive treatment at any empanelled hospital in India.
- It covers around 1,929 procedures, taking care of costs like drugs, diagnostic tests, doctor’s fees, room charges, and ICU expenses.
- Public hospitals are reimbursed for their services at the same rate as private hospitals.
List of Critical Diseases Covered Under Ayushman Bharat Yojana Scheme
The medical care scheme covers over 1,300 medical procedures at registered public and private hospitals across India. Some of the major illnesses covered under the Ayushman Bharat Yojana include:
- Double valve replacement
- COVID-19 treatment
- Prostate cancer
- Coronary artery bypass graft (CABG)
- Pulmonary valve replacement
- Anterior spine fixation
- Skull base surgery
- Laryngopharyngectomy with gastric pull-up
- Carotid angioplasty with stent placement
- Tissue expander for burn-related disfigurement
What is Covered Under PMJAY (Ayushman Bharat Yojana)?
Earlier government-funded health insurance schemes in India used to have coverage limits ranging from ₹30,000 to ₹3,00,000 per family, depending on the state, leading to a fragmented system. However, PMJAY offers a more unified approach by providing cashless coverage of up to ₹5,00,000 per eligible family per year for secondary and tertiary care.
The scheme covers all expenses related to:
- Medical exams, treatments, and consultations
- Pre-hospitalization care
- Medicines and medical supplies
- Intensive and non-intensive care
- Diagnostic tests and lab investigations
- Medical implants (if needed)
- Accommodation and food services
- Complications during treatment
- Follow-up care for up to 15 days after discharge
The ₹5,00,000 benefit is on a family floater basis, meaning any family member or multiple members can use it. Unlike the previous RSBY scheme, which had a five-member cap, PMJAY has no limits on family size or the age of members. Additionally, all pre-existing conditions are covered from the first day, so anyone with an existing health issue can get treatment as soon as they enroll in the scheme.
What are the Documents Required for Ayushman Bharat Yojana Scheme?
To apply for the PMJAY scheme, you’ll need the following documents:
- Proof of identity and age (such as Aadhaar Card or PAN Card)
- Contact details (mobile number, email address, and residential address)
- Caste certificate
- Documents showing your current family status
- Income certificate
Read more: How To Create Your ABHA Number on Paytm?
Eligibility Criteria for Rural and Urban Population
The PMJAY scheme aims to support the poorest 40% of India’s population, ensuring that only economically weaker and underprivileged sections benefit from it.
- PMJAY for Rural Population
The scheme covers rural households that meet at least one of the following six criteria:
- No adult members between the ages of 16 and 59.
- No adult male members between 16 and 59 years.
- Families belonging to SC/ST communities.
- Families living in a single room with kucha walls and roof.
- Households with disabled members and no able-bodied members.
- Landless families with manual labor as their main source of income.
2. PMJAY for Urban Population
For urban areas, eligibility is based on occupation, with 11 categories of workers covered, including:
- Domestic workers
- Beggars
- Ragpickers
- Construction workers (plumbers, masons, painters, etc.)
- Sanitation workers like sweepers and gardeners
- Cobblers, street vendors, and other service providers
- Shop assistants, peons, waiters, and delivery staff
- Chowkidars (guards) and washermen
- Artisans, tailors, and handicraft workers
- Drivers, rickshaw pullers, and helpers
How to Apply Online for Ayushman Bharat Yojana Scheme?
Step 1: Visit PMJAY official website: https://pmjay.gov.in/ and click on ‘Am I Eligible?’ on the top right hand corner of the homepage.
Step 2: Enter your details such as mobile number and authentication mode. Carefully enter the CAPTCHA code mentioned.
Step 3: Choose your state and search using your name, mobile number, Household ID (HHD) number, or ration card number.
Step 4: You can then check if you are eligible for the government healthcare scheme.
Check Your Eligibility for Ayushman Bharat PMJAY on Paytm App
Paytm, known for being the pioneer of digital payments and financial services, has integrated the Pradhan Mantri Jan Arogya Yojana (PMJAY) into its app. This allows users to check their eligibility and access health benefits, supporting the government’s goal of improving digital healthcare.
Paytm has made it easier for people to access various healthcare services. You can create a health ID, book teleconsultations, buy items from pharmacies, schedule lab tests, purchase health insurance, apply for medical loans, and more, all through Paytm.
Through the Paytm app, users can find a list of both private and government hospitals that participate in PMJAY. They can easily locate nearby hospitals covered by the scheme and use their phone to show their PMJAY health cover details to hospital staff.
Follow the given steps to check eligibility for Ayushman Bharat PMJAY on the Paytm app:
Step 1: Login to the Paytm App. Click on the search bar and type PMJAY.
Step 2: After clicking on the PMJAY icon, you can check your eligibility, find nearby hospitals and even call the helpline number directly from the Paytm app.
Step 3: Click on ‘check your eligibility’ and select your state from the drop down menu.
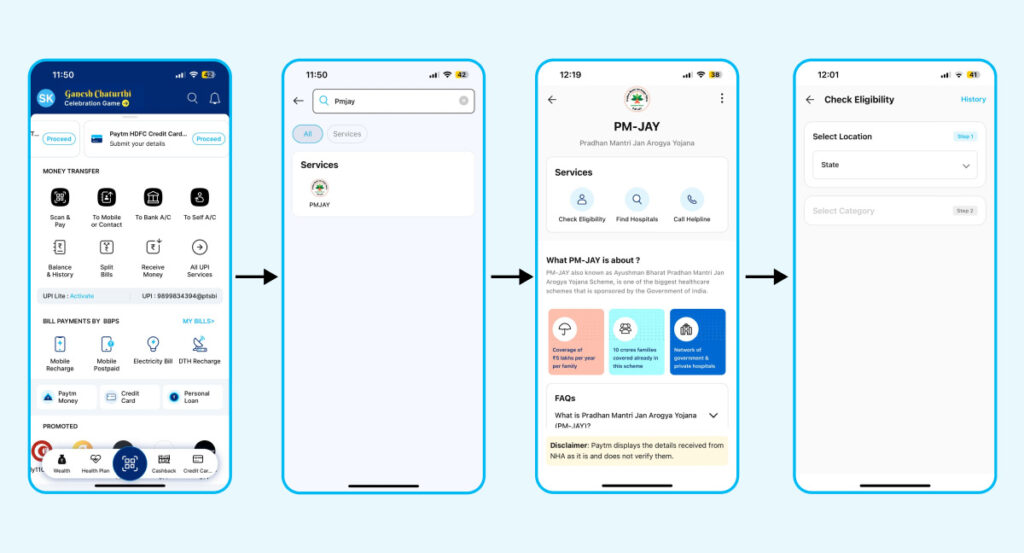
Step 4: Enter your details, including Name, Ration Card number, Household ID (HHD) number, mobile number, and other details.
What is Ayushman Card Under PMJAY?
The Ayushman Card is a key part of the Pradhan Mantri Jan Arogya Yojana (PMJAY), designed to offer health insurance coverage to Indian citizens, particularly those from vulnerable and economically weaker sections. This card acts as a tool for accessing healthcare services, making quality medical care more affordable and accessible.
How to Apply for Ayushman Bharat Card Online?
Follow the given steps to get Ayushman Bharat card online:
Step 1: After checking your eligibility, visit the official PMJAY website to start the online application.
Step 2: Click on the “ABHA Registration” button and use your Aadhaar card to begin the process.
Step 3: Enter the OTP sent to your phone to verify your Aadhaar.
Step 4: Provide other details such as your name, income, and PAN card information.
Step 5: Once your application is approved, you can return to the website and enter your Aadhaar number to generate an OTP.
Step 6: Use the OTP to download the digital copy of your Ayushman card.
Step 7: Print the card
Disclaimer: This blog is written to make it easy for readers to understand complicated processes. Some information and screenshots may be outdated as government processes can change anytime without notification. However, we try our best to keep our blogs updated and relevant.


